The three most common value leaks in hospitals—cancellations/no-shows, wait times, and coordination failures—aren’t “front-desk problems.” They’re symptoms of fragmented processes and data. A modern HIS (patient portal, EHR, telehealth, and interoperability) can close these gaps measurably when it’s designed with KPIs and clinical–IT governance.
1) Cancellations and No-Shows: From Friction to Engagement
- Patient portals. Having an active portal account at scheduling time is associated with 21 million fewer no-shows in 2024 and a 21.5% lower likelihood of missing visits. Embedding reminders, self check-in, and digital
payments in the portal reduces absences and speeds collections. ( Epic ) - Telehealth. In many specialties, remote visits show higher completion rates than in-person, especially for follow-ups. (PMC)
How the HIS enables this: scheduling with eligibility/prior-auth checks, secure messaging, multichannel reminders, one-click rebooking, and payment integrated to the chart.
KPIs: no-show rate by service, % rebookings via portal, average time-to-payment.
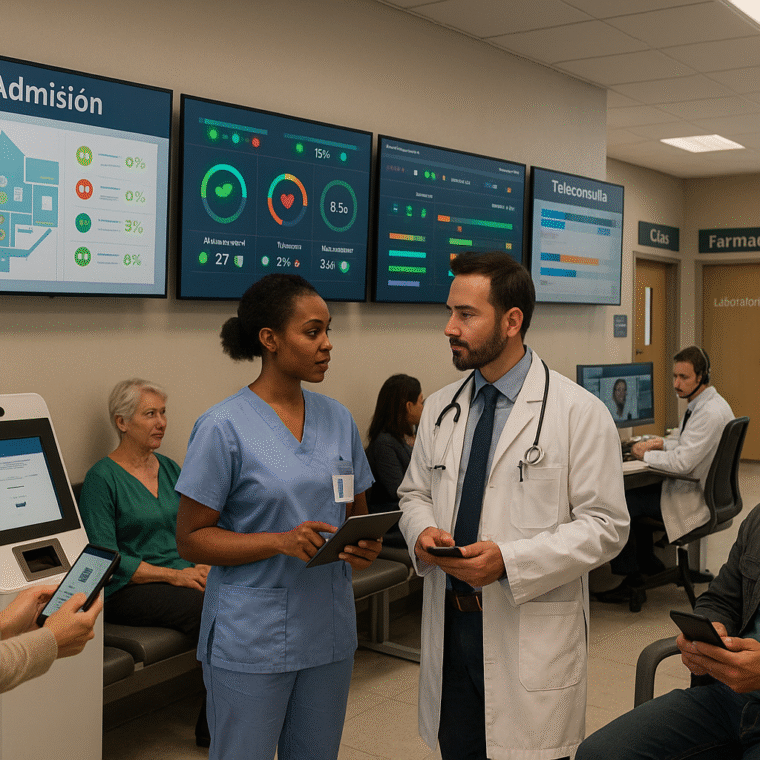
2) Wait Times and Patient Flow: See It, Predict It, Act
The crowding no es permanente; ocurre cuando la demanda supera capacidad de
How the HIS enables this: priority worklists, cycle-time dashboards (triage, door-to-doctor, door-to-discharge), long-stay alerts, and bed/transport coordination. Adding telehealth for timely referrals and online pre-admission reduces bottlenecks. (odphp.health.gov)
KPIs: door-to-doctor, LOS (case-mix adjusted), occupancy, % discharges before 11:00 a.m.
3) Clinical Coordination: Fewer Duplicates, Better Decisions
Interoperability (HIE/FHIR) prevents redundant tests and improves decision- making in urgent settings: studies report 9–25% reductions in duplicate imaging and savings near USD 2,000 per patient in some contexts. It can also lower LOS and 30-day readmissions when teams access the longitudinal record. (California
Health Care Foundation)
How the HIS enables this: HL7/FHIR connectors with lab, imaging, payers, and other providers; longitudinal viewers; closed-loop orders (request → perform → result → follow-up).
KPIs: % repeated studies, exchange latency/error rates, completeness of the clinical summary.
4) Documentation & AI: Remove Burden Without Losing Control
The Ambient AI scribes embedded in the EHR are associated with ~20% less time per note, ~30% less after-hours work, and higher same-day closure—freeing time for care coordination and reducing waits caused by paperwork. (JAMA Network)
In parallel, CDSS (allergy/interaction checks, reconciliation) prevents medication errors with up-to-date evidence; design and governance minimize alert fatigue. (NCBI)
KPIs: time in EHR per visit, % notes closed in-shift, ADEs per 1,000 patient-days,
acceptance of high-value alerts.
5) Governance & Public Policy: Conditions to Scale
Across the Americas, PAHO/OPS promotes maturity in Information Systems for Health (IS4H) and a Pan-American Digital Health “Highway” to strengthen governance, infrastructure, and workforce. That policy tailwind helps private hospitals pursue coordination and interoperability projects. (OPS)
Governance KPIs: data catalog coverage, effective interoperability (% complete, error-free messages), compliance with data policies.
Conclusion
Systemic inefficiencies aren’t solved by adding staff—they’re solved with visibility, rules, and closed-loop workflows. A modern HIS—plus portal and payments, telehealth, interoperability, and governed AI—recovers appointments, shortens waits, and synchronizes teams. The key is weekly measurement (no- shows, cycle times, duplicates, safety) and scaling what proves ROI.
¿Quieres verlo en tus propios flujos?
Agenda una demo de HarmoniMD + CLARA (el asistente médico con IA de HarmoniMD) o conversemos sobre tu proyecto para co-diseñar una ruta con KPIs claros para tu hospital.