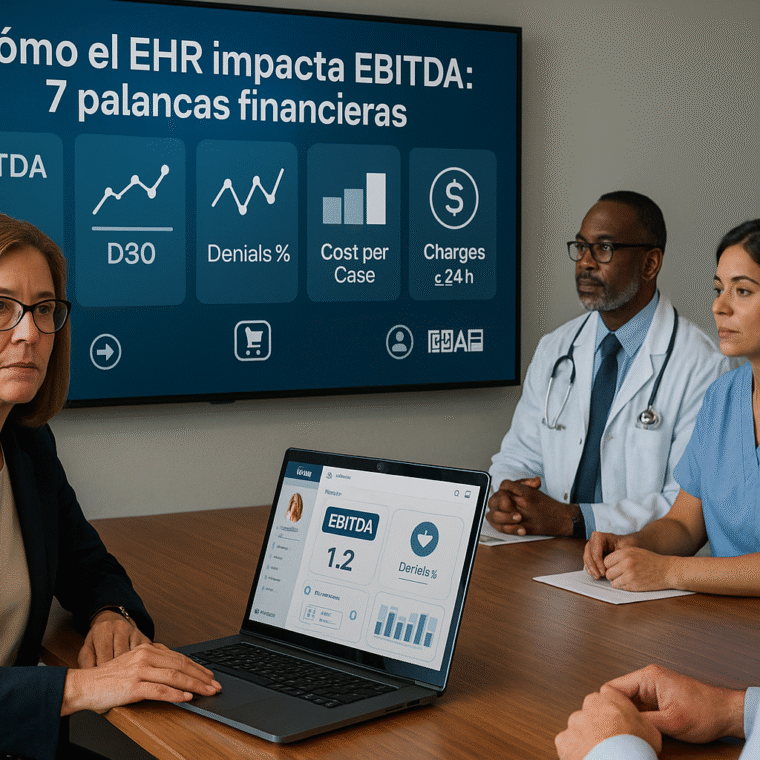
A well-implemented EHR moves the EBITDA needle in two ways: (1) revenue uplift (capture and collection) and (2) cost reduction (inefficiencies, adverse events, waste). Below are seven concrete levers—what they solve, how they impact results, and what to measure.
1) Revenue capture and CDI (Clinical Documentation Integrity)
What it solves: incomplete documentation → lower-severity codes → lower reimbursement.
How it impacts: Better documentation and AI/ambient scribe support improve note quality, reduce administrative burden, and enable more precise coding (MCC/CC), driving a higher case mix and stronger revenue. (PMC, JAMA Network)
Metrics: CDI query resolution rate, CMI, % diagnoses with MCC/CC, DRG weight variation.
2) Fewer denials and less RCM rework
What it solves: documentation/coding denials → lost revenue + reprocessing costs.
How it impacts: Denial management programs and root-cause analytics reduce first-pass rejections and accelerate cash-in. Data from 2024–2025 show growing denial pressure, so professionalizing this front has direct ROI. (American Hospital Association, Optum para Empresas, OncLive, OS Healthcare)
Metrics: initial denial rate, appeal overturn rate, cost per reworked claim, AR days by payer.
3) Fewer no-shows and omnichannel payments (patient portal)
What it solves: missed appointments and payment friction → schedule gaps and slow A/R.
How it impacts: Portal use is associated with fewer no-shows and—combined with omnichannel payments—speeds the revenue cycle. In 2024, an estimated 21 million fewer no-shows occurred among portal users. (Epic Research, beckershospitalreview.com)
Metrics: no-show rate by specialty, % rebookings via portal, average time to payment (from discharge), % digital payments.
4) Operational efficiency: LOS, throughput, and readmissions
What it solves: long stays and bottlenecks → lower bed turnover and higher cost.
How it impacts: EHR-integrated interventions and predictive models help reduce LOS and readmissions, improving operational performance without compromising safety. (JAMA Network, jmir.org)
Metrics: case-mix–adjusted LOS, 30-day readmissions, ED cycle time, service-level occupancy.
5) Interoperability that prevents duplicate spend
What it solves: repeated imaging/lab tests due to lack of shared information.
How it impacts: Data exchange (HIE/FHIR) is associated with 9–25% reductions in redundant imaging and savings near USD 2,000 per patient in certain contexts, freeing margin. (California Health Care Foundation)
Metrics: % repeated studies, exchange latency/error rates (HL7/FHIR), average cost per episode.
6) Medication safety and fewer adverse events
What it solves: prescribing/monitoring errors → longer stays, re-interventions, liability.
How it impacts: EHR-based interventions (CPOE, alerts, reconciliation) prevent errors and reduce adverse effects, with a direct cost impact. (ahrq.gov, PsNet)
Metrics: ADEs per 1,000 patient-days, complete reconciliation at discharge, clinical alert acceptance.
7) Supply costs and supply-chain resilience
What it solves: inflationary pressure and supply-chain disruption → thinner margins.
How it impacts: Fine-grained visibility of consumption/waste integrated into the EHR—plus supply analytics and material standardization—helps control one of the largest cost buckets in many hospitals; 2024–2025 continued to show cost tensions and shortages. (American Hospital Association, Premier, ghx.com)
Metrics: waste by service, cost per case (supplies), % standard formulary adoption, critical stockouts.
An EHR doesn’t improve EBITDA just by “having modules,” but by operating seven levers with discipline: precise documentation, fewer denials, portal/payments, operational efficiency, effective interoperability, medication safety, and supply control. The key is to prioritize 2–3 levers, set a baseline, measure weekly, and scale what proves return. With HarmoniMD, these levers become measurable workflows (dashboards, CLARA for documentation, patient portal, HL7 connectors) that turn the EHR from a data repository into a margin engine.