If the last few years taught us anything, it’s that digital maturity isn’t about “having
modules” it’s about operating a living system where data, people, and
processes flow securely and deliver outcomes. This blueprint summarizes the
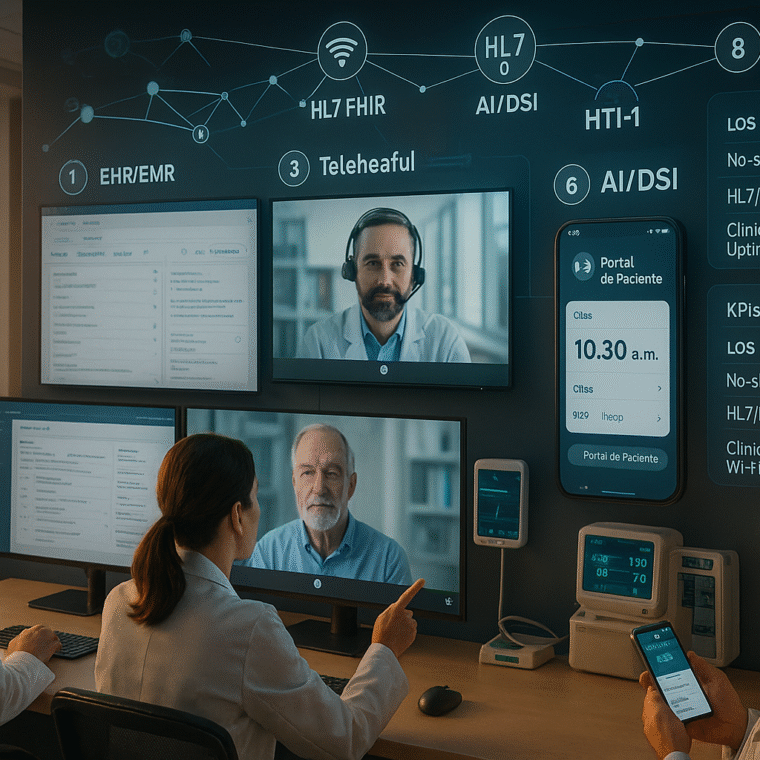
pillars (mHealth, EHR/EMR, telehealth, and wireless health), the minimum
architecture, and the KPIs that turn technology into clinical and financial value.
1) From vision to roadmap: what does “digital maturity” mean?
Reference models such as HIMSS Digital Health Indicator (DHI) and EMRAM
provide a practical compass to assess capabilities and plan staged evolution (0–7).
Using them as a framework prevents fragmented investments and helps prioritize
interoperability, analytics, and patient experience. (himss.org)
Roadmap tip: run a maturity assessment (DHI/EMRAM), define gaps, and
prioritize 90-day “quick wins” (e.g., portal + reminders + core KPIs) before tackling
larger changes.
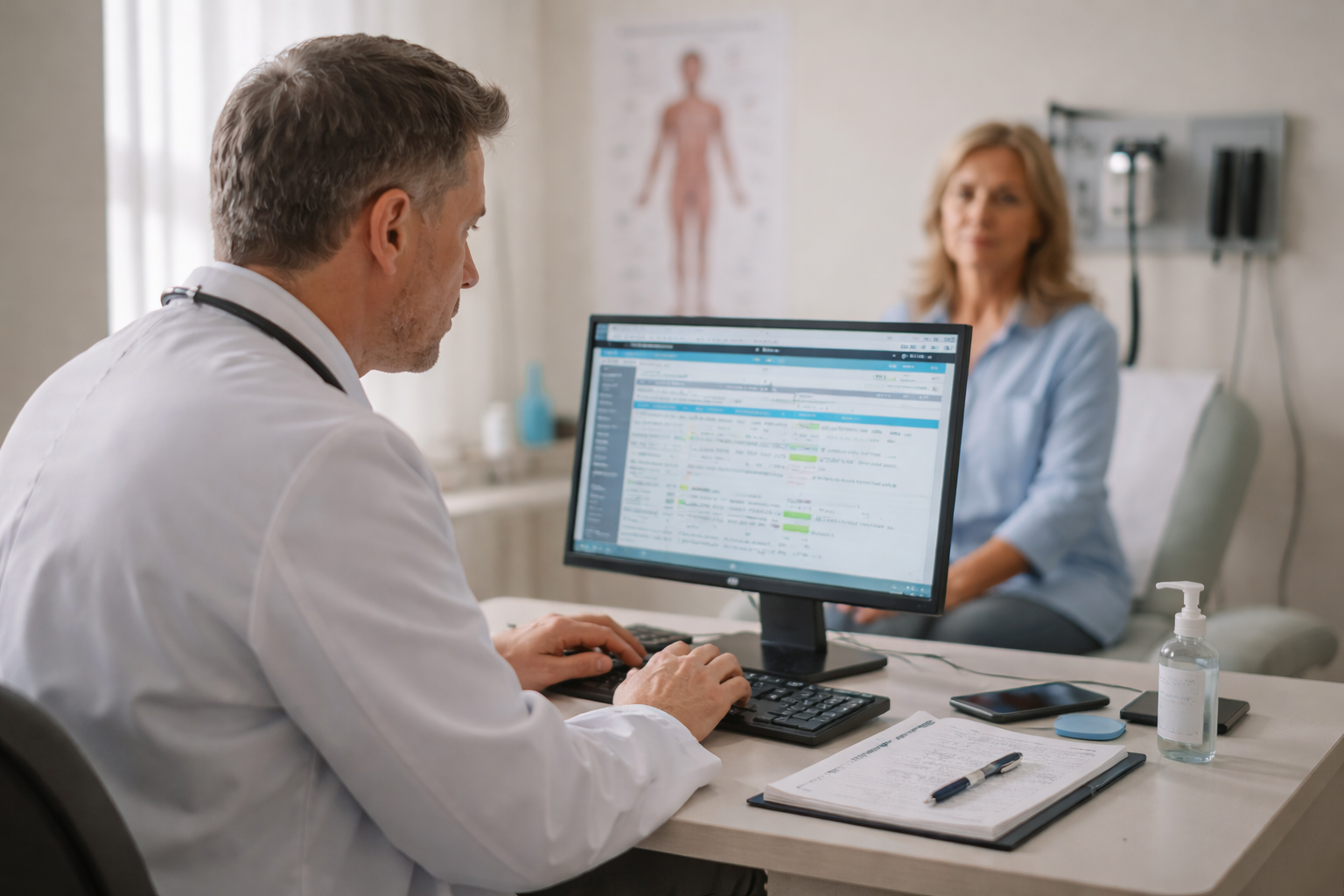
2) EHR/EMR pillar: the clinical nervous system
The EHR/EMR is the data and workflow backbone. In 2024, the US ONC HTI-1
rule strengthened algorithmic transparency for Decision Support Interventions
(DSI) and updated certification criteria (e.g., USCDI v3), raising the bar for safety
and explainability of AI inside the record. (healthit.gov, Federal Register)
What a mature operation requires:
- HL7/FHIR interoperability and exchange KPIs (latency, completeness,
errors). - Clinical–IT governance and actionable service dashboards (ED, inpatient,
OR). - DSI transparency (HTI-1): evidence-source attributes and recommendation
traceability. (healthit.gov)
3) Telehealth: hybrid continuity that scales access and quality
Telemedicine stabilized post-pandemic with sustained adoption in primary care
and behavioral health, acting as a substitute for some in-person care and
expanding access when properly integrated with the EHR and billing. (Alliance for
Connected Care)
ASPE/HHS briefings continue to document trends and population/service-level
utility—useful for planning coverage and payment. (aspe.hhs.gov)
Deployment checklist: video integrated into the chart, digital consents, linked
orders/notes, reminders, and KPIs (no-show, time-to-appointment, issue
resolution).
4) Mobile health (mHealth): del teléfono del paciente a datos accionables
The WHO Global Strategy on Digital Health (2020–2025) and recent guidance
emphasize that mHealth and other digital interventions must be grounded in
evidence, equity, privacy, and governance—moving from “apps” to programs
with measurable results. (Organización Mundial de la Salud, CNBIotecnología)
Good practices: authenticate the patient, standardize PROs (patient-reported
outcomes), connect mHealth → EHR → analytics, and measure adherence/clinical
impact.
5) Wireless health & devices: if the network fails, the flow fails
A robust wireless network isn’t a luxury: poor Wi-Fi degrades operational
efficiency and clinical experience, and today’s device density demands planning
(Wi-Fi 6/6E) and segmentation. (Cisco)
On security, the FDA and the Health Sector Coordinating Council (HSCC)
publish joint guidance and the Joint Security Plan for health delivery
organizations, while HC3 bulletins flag sector vulnerabilities. Maturity means
lifecycle security and incident response—not just “antivirus.” (U.S. Food and Drug
Administration, Consejo de Salud, HHS.gov)
For device-to-system interoperability at the bedside, the ISO/IEEE 11073 SDC
family (2024 editions) standardizes messaging and alerts across medical devices
and systems. (ISO, IEEE Standards Association)
6) The rules of the game: interoperability as public policy
The Interoperable Europe Act (in force since 11 April 2024) promotes cross-
border exchange and coordination among public administrations; while European,
its standards/governance logic inspire roadmaps elsewhere. (Interoperable Europe
Portal, Estrategia Digital Europa)
In the US, TEFCA (2023–2024) enabled nation-scale exchange and is evolving to support FHIR, setting the pace for “networks of networks” and
scalable APIs. (ASTP TEFCA RCE, CNBIotecnología)
7) Minimum viable architecture (Blueprint)
1. Clinical data layer (EHR/EMR) with HL7/FHIR and a data catalog.
2. Experience layer: patient portal, mHealth, telehealth—fully integrated.
3. Wireless/IoMT layer: segmented Wi-Fi 6/6E, device identity management,
continuous monitoring. (Cisco)
4. AI/DSI layer: clinical assistants with HTI-1 transparency, logged
recommendations, and impact metrics. (healthit.gov)
5. Governance & security: clinical–IT committee, incident response
(JSP/HC3), vendor management, and continuity drills. (Consejo de Salud,
HHS.gov)
8) KPIs that move the needle
- Clinical adoption: % electronic orders; note/sign time; in-shift note closure
rate. - Access & experience: no-show; time-to-appointment; portal NPS.
(aspe.hhs.gov) - Operations: LOS, occupancy, ED/OR throughput.
- Interoperability: HL7/FHIR latency/errors; message completeness.
- Wireless/IoMT: clinical Wi-Fi availability, SSID-level failures, device
inventory & patching. (Cisco) - Security/AI: mitigated incidents, response time, DSI transparency attributes
met. (healthit.gov)
Conclusion
Mature digital health happens when EHR/EMR, mHealth, telehealth, and
wireless operate as a measurable, secure system. Maturity frameworks
(HIMSS), interoperability rules (HTI-1, TEFCA, Interoperable Europe Act), and
security guidance (FDA/HSCC/HC3) have set the bar; now it’s about prioritizing use cases, governing AI with transparency, and sustaining weekly KPIs. Those
who do it accelerate access, elevate experience, and protect margins.
Want to see this applied to your reality?
Book a HarmoniMD + CLARA demo (HarmoniMD’s AI-powered medical
assistant), or let’s talk about your project and shape a path with clear clinical and
operational goals.